One of the reasons that women with PCOS seek help from GPs or hospital clinics is because of problems with skin which make them unhappy with their appearance. This is because of higher levels of hormones that are normally present at higher levels in men than in women, called androgens.
How can androgens affect the skin?
The skin can be affected in three ways:
- The growth of thicker hair (called terminal hair) in parts of the body where hair in women is usually fine; doctors call this hirsutism.
- Hair loss from your scalp, which could either be general thinning or loss of hair from around your forehead, called frontal balding. Some women are concerned about this. There are also other causes of this other than androgens.
- Acne may become more persistent and difficult to treat if you have PCOS. This is from increased oil production which is another way that androgens affect the skin.
How can the growth of unwanted thick hair (hirsutism) be assessed?
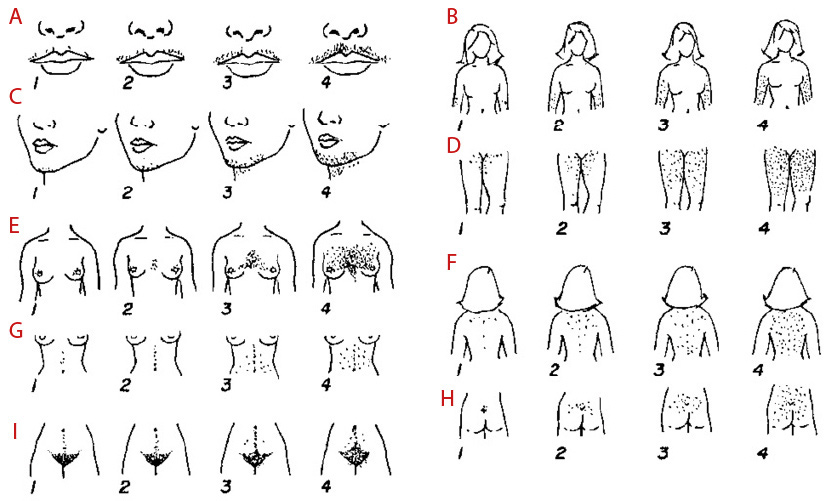
Add your score up here
If you scored 8 or more, this is clear evidence that you have what we call hirsutism. If you scored 3 or 4 in one area this may also be important for you and you may still want to consider treatment.
How can the growth of unwanted hair be managed?
While for some lifestyle change and weight loss may help in the long run, many will want to consider other options such as direct hair removal and medication. Opting for medication is worthwhile even if you opt for any form of direct hair removal including laser, as the medication can help to prevent regrowth and make your money go further.
Medications:
Important points:
- You should not get pregnant on any of the medications as it can affect the physical development of an unborn baby boy.
- Firstly, all medications take some time to work so you need to be patient. It may take 6-9 months before you start seeing a beneficial effect.
- All the medications work (on average your score can reduce by 7) but working may mean that you notice the hair is thinner or you have to remove it less often rather than the problem with hair completely disappearing, so expectations need to be realistic
- Unless anything else changes, such as your weight which may reduce the severity of the hormone imbalance and the androgen levels, when you stop the medication the problem with unwanted hair will return.
Combined Oral Contraceptive Pill
If you are able to have it, the combined oral contraceptive pill (COCP; contains oestrogen and a progestin), is the one to start with. The reason for this is that not only is it effective but different from other medications as it can help with irregular periods and prevents pregnancy.
How does it work?
- Oestrogen-containing oral contraceptives drive production of a protein called sex hormone binding globulin (SHBG) which mops up the androgens, thereby preventing them from acting on the hair follicles.
- In some COCP formulations, such as Yasmin or Dianette, the progestin component also works by blocking the action of androgens on the androgen receptor, thereby preventing androgens from exerting their effects on hair follicles.
What are the side effects?
The main risk of taking the combined oral contraceptive pill is the risk of blood clots in your leg veins or lungs. This risk is higher in those who are older, more overweight, smoke, have diabetes or hypertension and have a family history of clots. Women with migraines may not be able to have it. The risk of blood clots in women taking the combined oral contraceptive pill depends on the formulation used; for those on Yasmin, the risk is 10-12 per 10,000 patient years. This means that if 10,000 patients took Yasmin for 12 months, 10-12 of them would develop a blood clot. This compares with 5-7 per 10,000 patient years with other combined oral contracepives. The risk in those women who are not pregnant and not taking any pills is 2 per 10,000 patient years. Common side effects that you may experience can include nausea, bloating, breast tenderness, headaches, mood swings, and occasionally bleeding in between your periods. These can be discussed with your healthcare provider when considering treatment and these will be tailored to your own needs.
Antiandrogens
These medications can be added to the combined oral contraceptive pill either immediately, but usually after 6 months, or used alone when there is no chance of pregnancy (adequate alternative contraception or not sexually active or likely to become so). They are all equally effective. All antiandrogens described below have other uses and although frequently used in women with PCOS, they are not licensed for this. They work by reducing how much the hair is affected by the androgens.
Cyproterone acetate 50–100 mg a day on day 5-15 of menstrual cycle
It is well tolerated and side effects are rare. The only monitoring required is of liver function every now and then.
Spironolactone 100–200 mg a day in divided doses
This medication is normally used as a diuretic, so it may make you urinate more. Another potential side effect is dizziness. The drug is generally well tolerated but should not be used if your kidneys are impaired, although this scenario would be unusual in younger patients. If you are taking it with the combined oral contraceptive Yasmin, it is recommended that you have your kidney function checked after 4-6 weeks of treatment to check potassium levels.
Finasteride 2.5–5 mg a day
This is well tolerated with no adverse effects. A lower dose of 1mg is used in hair loss.
GnRH analogue therapy (Triptorelin intramuscular injection 3mg every 28 days)
This may be used in severe or resistant cases, and causes the reproductive hormones in the pituitary gland (FSH and LH) which stimulate the ovaries to be switched off. As this medication also causes oestrogen deficiency, it is vital that we use ‘add-back’ hormone replacement therapy (HRT) with oestrogen and progesterone to protect your bones, the lining of the womb and general health.
Other Treatments for Hair Loss & Acne:
The treatments listed above may also help with hair loss and acne if related to androgens. In the event that anti-androgen treatment is not successful, you may be referred to local dermatology departments where other treatments may be considered:
- Topical minoxidil for hair loss
- Benzoyl peroxide or long term antibiotics for acne. In severe cases, oral isotretinoin (Roaccutane) may be offered
- You will find useful information on the British Association of Dermatologists’ website (bad.org.uk) including information about acne www.acnesupport.org.uk.
Laser hair removal:
Laser hair removal is usually not funded by public health services but there may be variability in this between regions and countries.
Other forms of hair removal which offer less long term benefit are:
- Shaving which removes the hair at the level of the skin. It doesn’t change the shape of the hair in any way but it can give the appearance of looking thicker because of the blunt end.
- Plucking, waxing, threading, or mechanical devices removes the hair from just above the root where the hair grows from, and doesn’t result in a blunt end as shaving does. It is relatively safe but does cause some discomfort. Scarring and irritation can cause some changes in the colour of the skin particularly in women with darker skin.
- Creams containing chemical agents that dissolve hair are available. Once again, this may irritate the skin (especially on the face) which can cause some changes in colour.
Other options include:-
- Hair bleaching which may mask the appearance of darker hair. Once again, this may irritate the skin (especially on the face) which can cause some changes in colour.
- Epilation
- Electrolysis
- Vaniqa (eflornithine cream) is only for use on the face. It reduces the rate of hair growth and appearance of facial hair with noticeable results in 6-8 weeks. Side effects include skin irritation and acne.
This information leaflet has been co-authored by:
Dr. Michael O’Reilly (Consultant Endocrinologist, Beaumont Hospital)
Dr. Siona Ni Raghallaigh (Consultant Dermatologist, Beaumont Hospital)
Ms. Maureen Busby (CEO and Founder, PCOS Vitality patient support group https://www.pcosvitality.com/what-is-pcos)